Prostatitis, an inflammation of the prostate gland, is a common condition affecting millions of men worldwide. While many cases respond well to treatment, leaving prostatitis untreated can lead to serious and sometimes irreversible complications. Understanding the long-term effects of untreated prostatitis is crucial for men’s health, as early diagnosis and proper management can prevent lasting damage and improve quality of life. This article explores the types of prostatitis, the risks associated with neglecting treatment, and the importance of specialized care.
I. What Is Prostatitis?
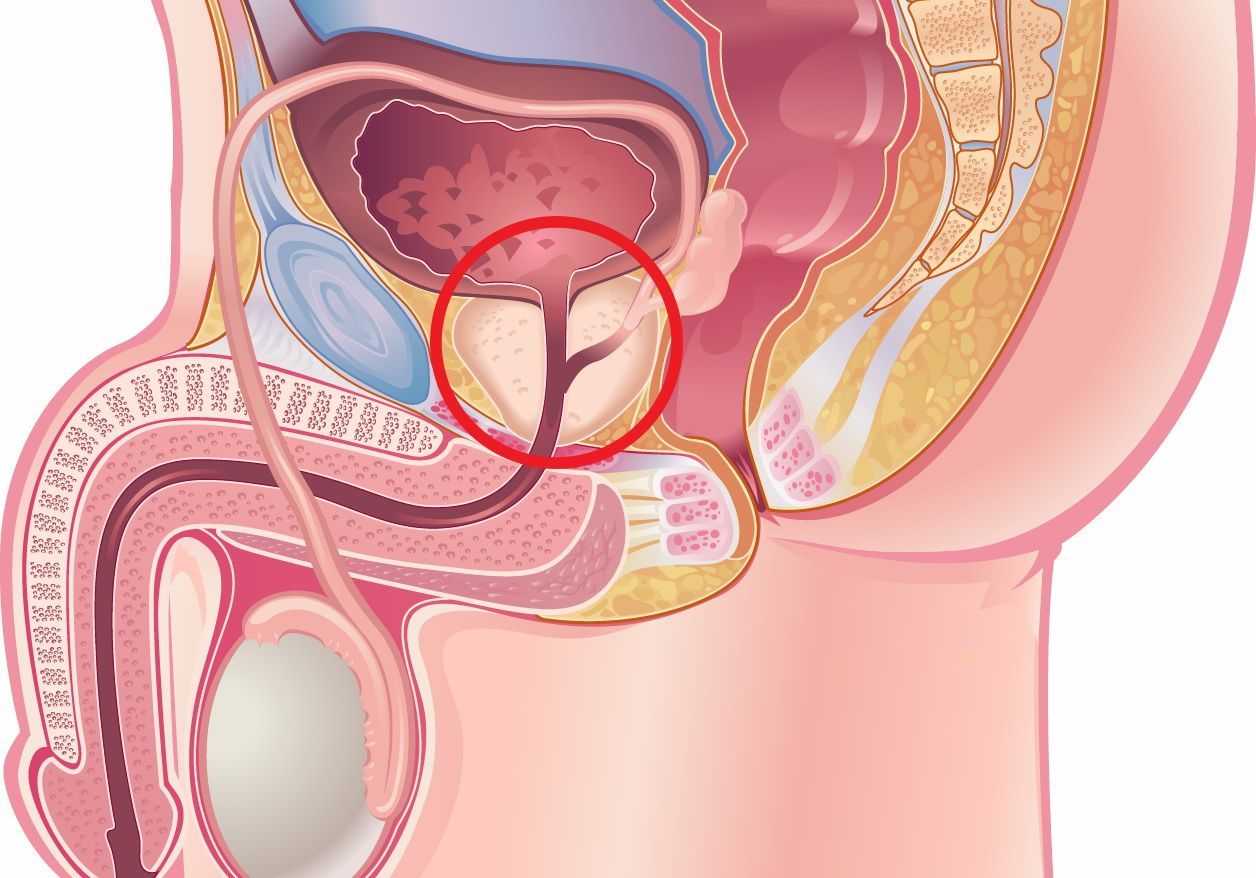
The prostate is a small gland located just below the bladder in men. It plays a vital role in reproductive health by producing seminal fluid, which nourishes and transports sperm. Prostatitis refers to inflammation of this gland and can be caused by bacterial infections or other non-infectious factors.
Prostatitis is classified into four main types:
- Acute Bacterial Prostatitis: A sudden bacterial infection causing severe symptoms such as fever, chills, and urinary difficulties. This form requires immediate medical attention.
- Chronic Bacterial Prostatitis: A persistent bacterial infection characterized by recurrent urinary tract infections and ongoing prostate inflammation.
- Chronic Nonbacterial Prostatitis/Chronic Pelvic Pain Syndrome (CPPS): The most common form, involving pelvic pain and urinary symptoms without detectable bacterial infection.
- Asymptomatic Inflammatory Prostatitis: Inflammation detected incidentally without symptoms, often during prostate cancer screening.
Symptoms of prostatitis vary but commonly include pelvic or perineal pain, urinary urgency and frequency, painful urination, painful ejaculation, and sexual dysfunction.
II. Why Is Untreated Prostatitis a Serious Concern?
Ignoring prostatitis or delaying treatment can lead to a range of serious long-term health problems. Due to the prostate’s central role in urinary and sexual function, chronic inflammation can cause significant complications affecting multiple systems.
1. Urinary Tract Complications
One of the most direct consequences of untreated prostatitis is progressive urinary tract dysfunction. Inflammation causes swelling and scarring of the prostate, which can obstruct urine flow through the urethra. This obstruction can lead to:
- Urinary Retention: Difficulty or inability to completely empty the bladder, sometimes requiring catheterization or emergency intervention.
- Recurrent Urinary Tract Infections (UTIs): Stagnant urine and bacterial colonization increase the risk of repeated infections.
- Bladder Dysfunction: Chronic obstruction causes the bladder muscle to thicken and lose elasticity, leading to symptoms like urgency, frequency, and incontinence.
- Kidney Damage: Severe or prolonged obstruction can cause urine to back up into the kidneys, increasing the risk of kidney infections (pyelonephritis) and potentially kidney failure.
2. Sexual Dysfunction and Quality of Life
Prostatitis can profoundly impact sexual health. Men with untreated prostatitis often experience:
- Erectile Dysfunction (ED): Difficulty achieving or maintaining an erection due to nerve irritation, pain, or psychological stress.
- Painful Ejaculation: Discomfort during or after ejaculation, which can reduce sexual desire.
- Reduced Libido: Chronic pain and emotional distress often diminish sexual interest and satisfaction.
Chronic pelvic pain syndrome (CPPS), in particular, is closely linked to sexual dysfunction and can severely impair quality of life.

3. Chronic Pain and Psychological Effects
Persistent pelvic pain is a hallmark of chronic prostatitis and CPPS. This pain can be debilitating, affecting daily activities, work productivity, and emotional well-being. Many men with untreated prostatitis suffer from anxiety, depression, and stress, which can exacerbate symptoms and create a vicious cycle of pain and psychological distress.
4. Risk of Prostatic Abscess and Systemic Infection
In cases of bacterial prostatitis, untreated infection may progress to form a prostatic abscess, a localized collection of pus within the prostate. This condition is serious and often requires surgical drainage. Furthermore, bacteria can enter the bloodstream, causing sepsis, a life-threatening systemic infection demanding urgent medical care.
5. Potential Link to Prostate Cancer
Emerging research suggests that chronic inflammation of the prostate, such as that seen in prostatitis, may increase the risk of prostate cancer. Chronic inflammation promotes oxidative stress and DNA damage, which can contribute to malignant transformation of prostate cells. A 2022 study published in Prostate Cancer and Prostatic Diseases reported that men with a history of prostatitis had nearly a threefold increased risk of developing prostate cancer compared to men without prostatitis.
III. How Is Prostatitis Diagnosed?
Early and accurate diagnosis is essential to prevent complications. Diagnosis typically involves:
- Medical History and Symptom Review: Detailed discussion of pain, urinary symptoms, and sexual health.
- Physical Examination: Including a digital rectal exam to assess prostate tenderness, size, and texture.
- Laboratory Tests: Urinalysis, urine culture, and sometimes semen analysis to detect bacterial infection.
- Imaging and Specialized Tests: Transrectal ultrasound or MRI may be used to identify abscesses or rule out other conditions. Urodynamic studies can evaluate bladder function if urinary symptoms are severe.
IV. Treatment and Management
1. Medical Treatments
- Antibiotics: The cornerstone for bacterial prostatitis treatment. Therapy often lasts several weeks to ensure eradication.
- Anti-inflammatory Medications: To reduce inflammation and relieve pain.
- Alpha-Blockers: These relax muscles in the prostate and bladder neck to improve urine flow and reduce urinary symptoms.
- Pain Management: Analgesics and neuromodulatory drugs may be used for chronic pain control.
2. Lifestyle and Supportive Therapies
- Pelvic Floor Physical Therapy: Helps relieve muscle tension and improve pelvic pain.
- Stress Reduction and Counseling: Psychological support can address anxiety and depression linked to chronic prostatitis.
- Dietary Modifications: Avoiding bladder irritants such as caffeine, alcohol, and spicy foods may reduce symptoms.
- Regular Exercise: Improves overall health and may alleviate symptoms.
3. Importance of Follow-Up
Regular follow-up appointments are critical to assess treatment effectiveness, monitor for complications, and adjust therapy as needed.

V. The Role of Men’s Health Vietnam Center in Prostatitis Care
Men’s Health Vietnam center provides specialized, multidisciplinary care tailored to men’s urological and sexual health needs. Their services include:
- Advanced Diagnostic Testing: To accurately classify prostatitis and identify complications.
- Personalized Treatment Plans: Combining antibiotics, physical therapy, pain management, and psychological support.
- Sexual Health Management: Addressing erectile dysfunction and painful ejaculation associated with prostatitis.
- Patient Education: On lifestyle changes and preventive measures to support prostate health.
At the Men’s Health Vietnam center, patients benefit from a holistic approach that addresses both physical symptoms and emotional well-being, aiming to restore function and improve quality of life.
- Address: 7B/31 Thanh Thai Street, Ward 14, District 10, Ho Chi Minh City, Vietnam
- Website: menhealth.vn
- Fanpage: facebook.com/trungtamsuckhoenamgioi
- Contact: (+84) 902 353 353
 0902 353 353
0902 353 353 Giờ làm việc: 08:00 - 20:00
Giờ làm việc: 08:00 - 20:00 7B/31 Thành Thái, Phường Diên Hồng, TP. HCM
7B/31 Thành Thái, Phường Diên Hồng, TP. HCM
