Chronic prostatitis, particularly chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), is a widespread yet frequently overlooked condition that affects millions of men globally. While often dismissed as a minor urological issue, chronic prostatitis poses a significant silent threat to men’s sexual health, profoundly impacting quality of life, intimate relationships, and psychological well-being. This comprehensive article delves into the epidemiology, symptoms, diagnosis, and treatment of chronic prostatitis, emphasizing its connection to sexual dysfunction. Drawing on authoritative medical literature and recent research, it also highlights the critical role of specialized men’s health clinics in managing this complex condition.
I. Understanding Chronic Prostatitis: Definition and Epidemiology
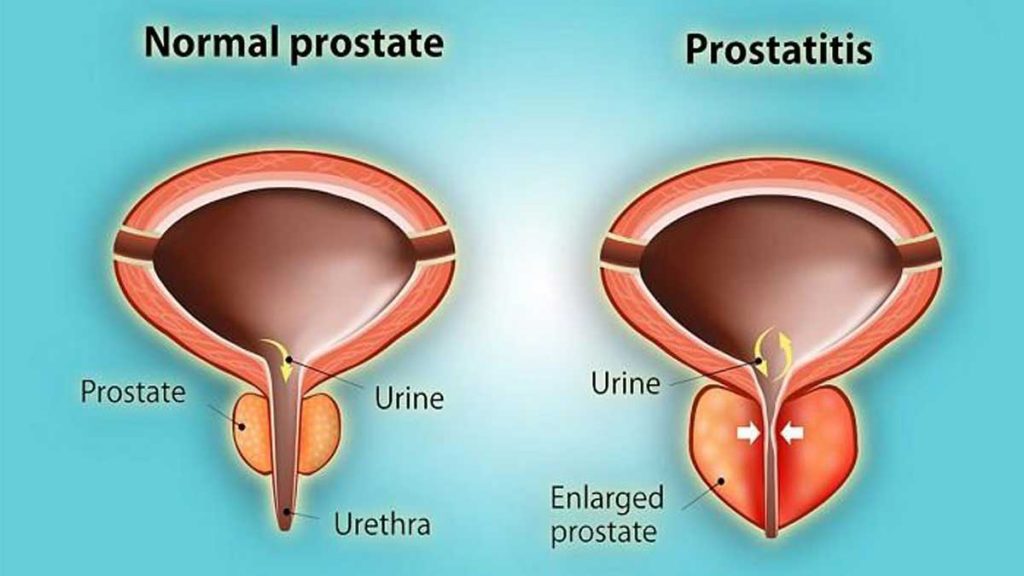
Chronic prostatitis is an umbrella term describing persistent inflammation or discomfort of the prostate gland lasting at least three months. It is classified into four categories by the National Institutes of Health (NIH):
- Category I: Acute bacterial prostatitis
- Category II: Chronic bacterial prostatitis
- Category III: Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), subdivided into IIIa (inflammatory) and IIIb (non-inflammatory)
- Category IV: Asymptomatic inflammatory prostatitis
Of these, CP/CPPS (Category III) is the most common and clinically challenging form, accounting for approximately 90-95% of prostatitis cases seen in urology clinics worldwide (Nickel et al., 2021).
II. Prevalence and Impact
Studies estimate that up to 8.4% to 25% of men experience symptoms consistent with chronic prostatitis during their lifetime (Zhang et al., 2020). CP/CPPS affects men across all age groups but is most prevalent in men aged 35 to 50. Despite its high prevalence, many men do not seek medical help due to stigma, embarrassment, or the intermittent nature of symptoms, contributing to underdiagnosis and undertreatment.
III. Symptoms and Clinical Presentation
1. Core Symptoms
Chronic prostatitis manifests with a constellation of symptoms that vary widely in severity and duration. The primary complaints include:
- Chronic pelvic pain: Persistent discomfort localized to the perineum, lower abdomen, groin, or lower back lasting more than three months.
- Urinary symptoms: Increased frequency, urgency, dysuria (painful urination), and nocturia.
- Sexual dysfunction: Painful ejaculation, erectile dysfunction (ED), premature ejaculation (PE), and decreased libido.
- Psychological distress: Anxiety, depression, and stress often accompany the physical symptoms, exacerbating the overall burden.
2. Diagnostic Challenges
Diagnosing CP/CPPS is complex due to the absence of definitive biomarkers or imaging findings. The diagnosis is primarily clinical, based on symptom history and exclusion of other causes such as urinary tract infections, sexually transmitted infections, or malignancy.
The National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) remains the gold standard for assessing symptom severity and impact on quality of life. It evaluates pain, urinary symptoms, and quality of life domains, providing a standardized approach to diagnosis and monitoring.

IV. The Link Between Chronic Prostatitis and Sexual Dysfunction
1. Prevalence of Sexual Dysfunction in CP/CPPS
Sexual dysfunction is a common but often underreported consequence of chronic prostatitis. A comprehensive meta-analysis involving over 11,000 men with CP/CPPS revealed:
- Overall sexual dysfunction prevalence: Approximately 62%
- Erectile dysfunction prevalence: Around 29%
- Premature ejaculation prevalence: Approximately 40%
Interestingly, while overall sexual dysfunction rates have shown a slight decline over recent years, the prevalence of erectile dysfunction among these patients has been increasing (Cui et al., 2015; Zhang et al., 2015).
2. How Does Chronic Prostatitis Affect Sexual Health?
The mechanisms linking chronic prostatitis to sexual dysfunction are multifactorial and not yet fully elucidated. Key contributing factors include:
- Chronic pain and inflammation: Persistent pelvic pain can interfere with sexual arousal and performance.
- Pelvic floor muscle dysfunction: Hypertonicity or spasm of pelvic muscles can cause painful intercourse and erectile difficulties.
- Neurogenic and vascular factors: Inflammation may impair nerve signaling and blood flow essential for erection.
- Psychological factors: Anxiety, depression, and stress related to chronic pain and sexual difficulties further exacerbate dysfunction.
Men with CP/CPPS often report painful ejaculation, difficulty achieving or maintaining erections, reduced sexual desire, and diminished satisfaction, all of which significantly impair quality of life and intimate relationships.
V. Current Approaches to Management
1. Pharmacological Treatments
Treatment of chronic prostatitis and associated sexual dysfunction is challenging and often requires a multimodal approach:
- Antibiotics: Reserved for confirmed bacterial prostatitis (Categories I and II); their role in CP/CPPS remains controversial.
- α-Blockers: Used to relieve urinary symptoms by relaxing smooth muscle in the prostate and bladder neck.
- Anti-inflammatory agents: Nonsteroidal anti-inflammatory drugs (NSAIDs) may reduce pain and inflammation.
- Neuropathic pain medications: Gabapentinoids and tricyclic antidepressants can help manage chronic pelvic pain.
- Phosphodiesterase-5 inhibitors (PDE5i): Sildenafil and tadalafil improve erectile function and may have ancillary benefits on pelvic blood flow and pain.
2. Non-Pharmacological and Supportive Therapies
- Pelvic floor physical therapy: Targeted exercises and biofeedback help relieve muscle spasm and improve pelvic function.
- Psychological counseling: Cognitive-behavioral therapy (CBT) addresses anxiety, depression, and coping strategies.
- Lifestyle modifications: Stress reduction, regular exercise, dietary adjustments, and smoking cessation can improve symptoms.
- Alternative therapies: Acupuncture and heat therapy have shown some benefit in symptom relief.

VI. Multidisciplinary Care
Given the complexity of CP/CPPS, a multidisciplinary approach involving urologists, pain specialists, physiotherapists, and mental health professionals is considered best practice. This coordinated care improves symptom control, sexual function, and overall quality of life.
VII. The Role of Men’s Health Vietnam Center in Managing Chronic Prostatitis
Men’s Health Vietnam Center plays a pivotal role in the comprehensive management of chronic prostatitis and its sexual health implications. These specialized centers offer:
- Expert urological evaluation: Advanced diagnostic tools including uroflowmetry, prostate imaging, and laboratory testing.
- Personalized treatment plans: Tailored therapies addressing both prostatitis symptoms and sexual dysfunction.
- Integrated sexual health services: Counseling, medication management, and rehabilitation for erectile dysfunction and other sexual concerns.
- Psychological support: Access to mental health professionals skilled in managing chronic pain and its psychological sequelae.
- Patient education and support: Empowering men with knowledge and coping strategies to manage their condition effectively.
At facilities like the Men’s Health Vietnam Center, patients receive holistic care that addresses the physical, psychological, and sexual dimensions of chronic prostatitis, leading to better outcomes and improved quality of life.
- Address: 7B/31 Thanh Thai Street, Ward 14, District 10, Ho Chi Minh City, Vietnam
- Website: menhealth.vn
- Fanpage: facebook.com/trungtamsuckhoenamgioi
- Contact: (+84) 902 353 353
 0902 353 353
0902 353 353 Giờ làm việc: 08:00 - 20:00
Giờ làm việc: 08:00 - 20:00 7B/31 Thành Thái, Phường Diên Hồng, TP. HCM
7B/31 Thành Thái, Phường Diên Hồng, TP. HCM
